Complementary feeding: what, when and how
Currently there is a wide range of guides and documents on infant feeding, but doubts among parents are increasing, mainly due to the variety and disparity of information. Recommendations from the pediatric population differ in some cases on the form and age of introduction of foods , to which we add the great influence that has Internet , the social networks with tips “no health professionals” and view family and friends , which can lead to some confusion . For all this, it is of great interest to resolve doubts and make known what the current situation is regarding complementary feeding (CA): when to start, what foods to include or not and in what order.
Index of contents
- 1 Definition and objectives
- 2 When to start?
- 3 “Sorting” food
- 4 Potentially allergenic foods?
- 5 What about gluten?
- 6 Should some foods be avoided?
- 7 Conclusions
Definition and objectives
The term of German origin “beikost” introduced by Fomon was proposed by the Anglo-Saxons in the 1950s to designate any kind of food used in infant feeding, other than human milk or formula 1 . First of all, we must know what are the objectives of the introduction of this type of diet 2 :
- Provide an adequate diet that meets the nutritional requirements of the child for optimal growth and development.
- Develop good habits that in the future prevent obesity, poor teeth, diabetes, and cardiovascular diseases.
- Provide a balanced and complete diet that avoids specific nutrient deficiencies (iron, zinc, calcium, vitamin A and D).
- Development of taste and palatability: different textures, smells and flavors since this is the basis for a healthy diet in the not too distant future.
When to start?
There is an impossibility in establishing strict feeding standards about when is the best time to introduce complementary foods into the infant’s diet. The World Health Organization (WHO) and the United Nations Children’s Forum (UNICEF) recommend maintaining exclusive breastfeeding for the first six months of life and therefore, CA thereafter 3,4 .
Some authors indicate its onset at 6 months of life for those who are exclusively breastfeeding (BF) and between the fourth and sixth month for those who take artificial or mixed breastfeeding, although there is no clear consensus in the scientific literature for the latter 5.6 . Others do not differentiate between types of breastfeeding, but they do make it clear that it should not be introduced before 4 months and in all cases it should have started at 6 months of age 7,8 . Speaking of weeks, the Nutrition Committee of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition ( ESPGHAN ) indicates that CA should not be introduced before 17 weeks or later than 26 weeks, assessing in each child individually their nutritional capacities and the characteristics of their neurological development 8 .
The latest scientific opinion of the European Food Safety Authority (EFSA) “Appropriate age range for the introduction of complementary feeding in the baby’s diet” indicates that there is no conclusive evidence that there are neither harms nor benefits in its introduction before the 6 months, with the exception of infants at risk of iron depletion (exclusively breastfed infants whose mothers have low iron levels, those with early umbilical cord clamping, premature infants, infants small for gestational age, and those with high rate of growth) that could benefit 9 .
But even with all this, BA should not begin until the baby is “ready”: acquire the psychomotor skills that allow safe handling and swallowing (sitting with support, disappearance of the extrusion reflex) and an active interest in try new flavors and textures 5.10 .
“Sorting” food
Although there are no reasons that justify the specific order of introducing foods in the infant’s diet , it is important to prioritize those with high iron content since, at 6 months of age, the endogenous iron stores of the baby are depleted and the The need for exogenous iron increases rapidly as the physiological requirement per kg of body weight becomes higher than in other stages of life 8 . After the sixth month, 90% of the iron required by babies with SCI must come from AC 6 .
Guidance proposals are included within the different food introduction calendars that must be adapted according to the family reality, in order to progressively incorporate the baby into the family’s diet 11 .
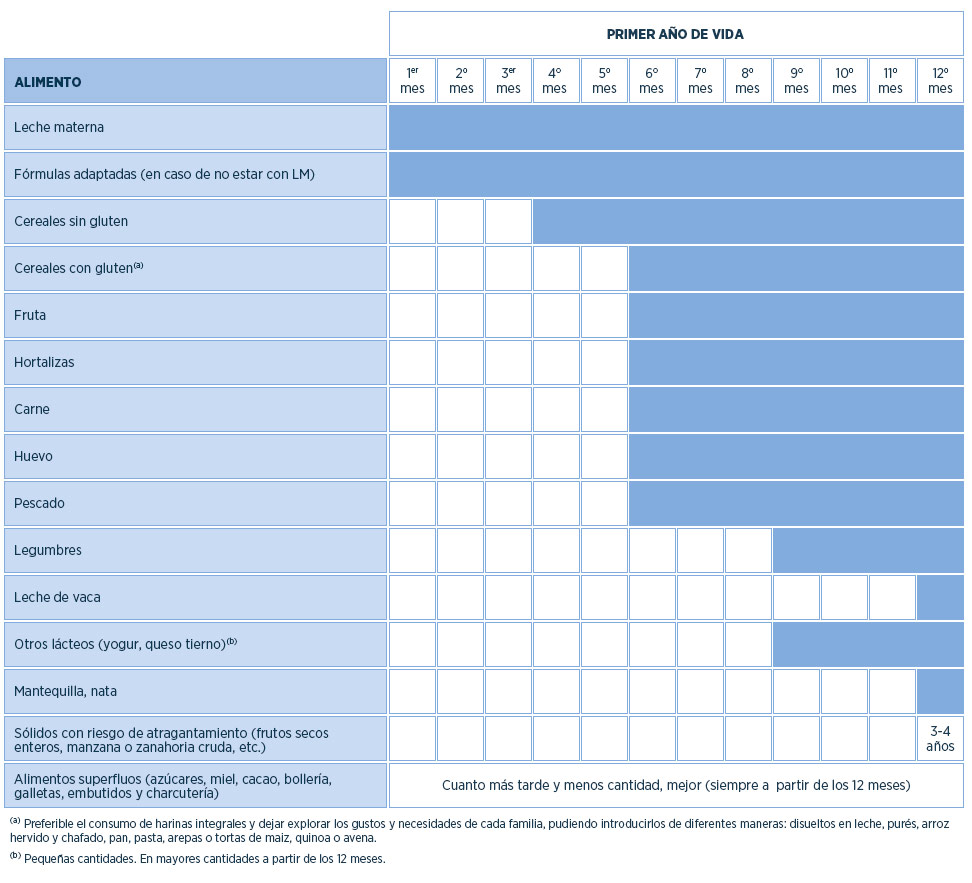
Table 1. Indicative food introduction calendar
Source: Own elaboration from the following sources 5,10-14
Potentially allergenic foods?
Delaying the introduction of certain foods appears to be unrelated to allergy prevention 7 . Already in 2008 it was confirmed that there was no convincing scientific data to justify the delay in the introduction of foods with potential allergenicity after 6 months to protect against allergic diseases 15,16 . Currently, this statement continues to be valid 6,8,9,17 , adding that it is independent of the type of atopy that the person suffers 18 .
In the work of Ferraro, Zanconato and Carraro (2019) it is concluded that “the available studies suggest that the introduction of allergenic foods should not be postponed after 4 to 6 months of age, both in high-risk and low-risk infants”. However, based on existing data, the only clear recommendation refers to the early introduction of peanuts between 4 and 11 months of age as a preventive measure to reduce food allergies in high-risk babies, even if safety and feasibility of doing so has yet to be fully explored 19 . ESPGHAN also confirms this, highlighting that there is close pediatric supervision 8 .
When introducing new foods to your baby’s diet, the American Academy of Pediatrics (AAP) and the Centers for Disease Control and Prevention (CDC) recommend waiting 3 to 5 days between introducing new foods in complementary feeding to monitor possible allergic reactions 20-22 .
What about gluten?
The introduction of gluten before 4 months is not recommended and it is recommended to introduce it around 6 months and gradually 7 . The Ribes et al. prepared a consensus document based on scientific evidence in 2015 to establish the recommendations for the introduction of gluten 23 .
1. SCI is always recommended, regardless of its effect on the development of Celiac Disease (CD).
2. It is recommended to introduce the AC preferably while maintaining the LM.
3. The introduction of gluten before 4 months of age is not recommended .
4. It is recommended to introduce gluten around 6 months of age :
-
-
- Its introduction between 5-6 months seems a reasonable option.
- If for any reason CA starts early, eventually it could be considered to introduce it after 4 months, although at that age other cereals, such as corn or rice, not related to CE could be used.
- In the event of a delay in the introduction of CA, the inclusion of gluten could be delayed without posing an additional risk to the patient with respect to the possible development of CD.
-
5. Introduce gluten in small quantities: you can start with 1-2 scoops of cereals or a cookie a day.
6. Once introduced, increase its consumption gradually depending on the nutritional needs (caloric intake) and the infant’s tolerance.
The recommendation of the ESPGHAN in its position of the year 2016 is to introduce gluten between 4 and 12 months of age and in small quantities at the beginning . The age of introduction of gluten in infants of this range does not seem to influence the absolute risk of developing CHD in children 24 .
Finally, the EFSA published in 2019 the scientific opinion “Appropriate age range for the introduction of complementary feeding in the baby’s diet” 9 in which it says that there is not enough evidence to affirm that introducing gluten in children under 6 months compared to those older than that age increases the risk of developing CD. Gluten can be introduced at the same time as the rest of complementary foods .
Should some foods be avoided?
There are certain foods that cannot be introduced into the infant’s diet until at least 12 months. Those foods rich in arsenic (from growing waters), such as rice bran and rice drinks 8 . The algae must also be avoided because of its high iodine content and foods with laxative effect as chia seed flax and 25 . Do not introduce the honey until after 12 months, due to the risk of containing spores of Clostridium Botulinum 6,12,25 . The fennel not be introduced until 4 years because it contains estragole 8 .
It is recommended to delay until 12 months the introduction of green leafy vegetables (chard, spinach, borage), beets and turnip , due to their high nitrate content (and if they are used, they do not account for more than 20% of the total content of the dish ), whose presence increases even more with the conservation time of the food once it is prepared. This increase in nitrates leads to an increased risk of methemoglobinemia in younger children 5 , which is why pureed vegetables should be kept in a refrigerator for a maximum period of 24 hours, and can also be frozen if they are not consumed. same day 12 .
Due to this, the Spanish Agency for Food Safety and Nutrition (AESAN) has recently published some recommendations that include information on the time of introduction of chard, spinach and borage in infant food 26 .
Also avoid foods that can cause choking : whole nuts (offer them crushed), popcorn, whole grapes, whole carrot or apple or large pieces, cross-cut sausages, sweets, etc. 5,10,17 .
Regarding the presence of methylmercury, AESAN has made some recommendations for fish consumption , advising vulnerable populations (pregnant women or planning to be pregnant, lactating or children from 0 to 10 years) on the preferential consumption of certain species with low and medium mercury content and avoid other species with high content, such as: swordfish / emperor, bluefin tuna (Thunnus thynnus), shark (dogfish, porbeagle, dogfish, dogfish and blue shark) and pike 27 .
Furthermore, because of the presence of cadmium, children should avoid the regular consumption of shrimp heads, prawns and crayfish or the body of crab-like crustaceans 12 .
Breast milk and infant formulas have the necessary amount of salt. Infants need a very small amount since their kidneys are too immature, so salt should not be added to babies’ AC, even if it is tasteless 5 . In addition, foods such as dried soups, bouillon cubes, cured meats, precooked meats, and canned vegetables should be avoided 6,11 .
Nor is it appropriate to sweeten with sugar, honey, condensed milk or sweeteners , which will predispose to an early appetite for sweets, and also increases the risk of cavities, diabetes and obesity 14 . Various scientific societies recommend avoiding added sugars in the diet of infants and young children 8,28,29 . The AAP advises avoiding fruit juices in children under the age of 30 .
Avoid the consumption of viscera and offal (liver, kidneys, heart …) due to the risk of contribution of parasites, toxins and hormones, and an excessive amount of fat and cholesterol for the infant 6 . Children under 6 years of age should not consume meat from animals hunted with lead ammunition because it causes neuronal damage 12 .
Conclusions
There are no exact dates to start CA, but it can be confirmed that this is not before 4 months or after 6, since from then on the BF is insufficient to cover the requirements of certain nutrients (for example the iron). There is also not enough scientific evidence on the benefits of introducing foods in a specific order or chronology, 7 so the most current and contrasted recommendations in different epidemiological studies should be followed and we must forget about previous schemes that, on many occasions, lead to confusion among patients. parents. What it is necessary to remember and apply is the recommendation of exclusive breastfeeding up to 6 months of age 3,31 .
It is essential to maintain continuous communication between the family, the Pediatric team and the Dietitian-Nutritionist without “instilling” rigid rules in the incorporation of new foods, but must be personalized , according to the development and characteristics of the baby, tastes family and food availability, always following evidence-based guidelines.






















+ There are no comments
Add yours